Urodynamic Testing: When and Why Is It Necessary for Diagnosis and Treatment?

Urodynamic testing is a vital component of urologic healthcare, providing valuable insights into the function of the lower urinary tract. By assessing bladder and urethral dynamics, urodynamic testing aids in diagnosing and treating various urological conditions. This article presents a thorough overview of urodynamic testing, covering its different types, indications, advantages, preparation, and interpretation of test results.
What is Urodynamic Testing?
Urodynamic testing involves a series of procedures assessing the urinary system’s function and coordination. It provides detailed information about bladder capacity, pressure, urine flow rates, and muscle activity. Various types of urodynamic tests are employed to evaluate specific aspects of urinary function:
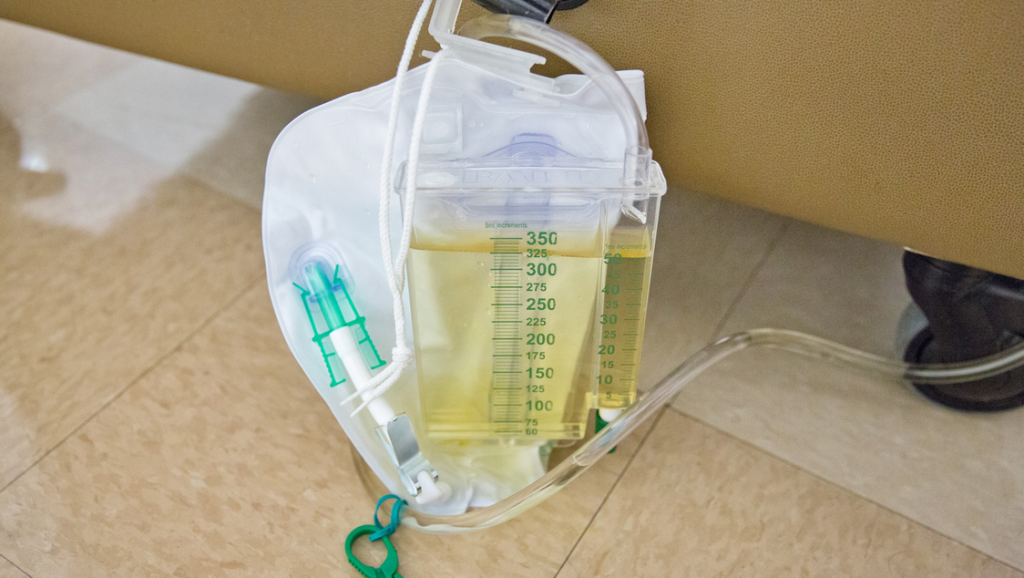
Uroflowmetry: Measuring Urine Flow
Uroflowmetry measures the rate and volume of urine flow during voiding. It helps identify abnormalities in urine flow patterns and can be an initial screening test for lower urinary tract dysfunctions.
Cystometry: Evaluating Bladder Function
Cystometry assesses bladder filling and emptying by measuring pressure changes. It aids in diagnosing overactive or underactive bladder, bladder outlet obstruction, and other bladder-related disorders.
Electromyography: Assessing Muscle Activity
Electromyography (EMG) measures the electrical activity of the muscles involved in urinary control. It aids in evaluating neurogenic bladder conditions and detrusor sphincter dyssynergia.
Pressure Flow Study: Assessing Voiding Mechanics
A pressure flow study evaluates the pressure within the bladder and urine flow during voiding. It helps diagnose bladder outlet obstruction and detrusor underactivity.
Video Urodynamic Tests: Visualizing the Urinary Tract
Video urodynamic tests combine imaging techniques, such as fluoroscopy or ultrasound, with conventional urodynamic procedures. They provide a dynamic visualization of the urinary tract during filling and voiding.
Indications for Urodynamic Testing
Urodynamic testing is indicated in various clinical scenarios:
1. Lower Urinary Tract Symptoms (LUTS)
Lower urinary tract symptoms encompass a range of bothersome urinary complaints. Urodynamic testing is particularly useful in identifying the underlying causes of LUTS, including:
- Urinary Incontinence: Urodynamic testing helps determine the type of urinary incontinence, such as stress incontinence (leakage with physical activities) or urge incontinence (sudden strong urge to urinate leading to leakage). This information assists in tailoring appropriate treatment strategies.
- Urinary Frequency and Urgency: Urodynamic evaluation aids in distinguishing between bladder-related causes, such as overactive bladder, and non-bladder causes for urinary frequency and urgency. It helps guide targeted interventions to alleviate these symptoms.
- Urinary Retention: Urodynamic testing can identify the presence of incomplete bladder emptying or urinary retention. This information is essential for determining appropriate management approaches, such as intermittent catheterization or medication therapy.
- Nocturia: Nocturia, the need to wake up during the night to urinate, can have various underlying causes. Urodynamic testing helps evaluate bladder function and nocturnal urine production, contributing to an accurate diagnosis and targeted treatment.
- Hesitancy and Weak Urine Stream: Urodynamic testing assists in assessing bladder contractility and the presence of bladder outlet obstruction, which can contribute to hesitancy and a weak urine stream. It aids in identifying the appropriate interventions, such as medication or surgical procedures, to alleviate these symptoms.
2. Neurological Disorders Affecting Bladder Function
Patients with certain neurological conditions often experience bladder dysfunction. Urodynamic testing is valuable in evaluating bladder function and guiding management in the following disorders:
- Multiple Sclerosis: Urodynamic testing helps assess neurogenic bladder dysfunction in patients with multiple sclerosis. It aids in determining the appropriate interventions to manage symptoms such as urinary urgency, frequency, and incontinence.
- Parkinson’s Disease: Urodynamic evaluation assists in detecting changes in bladder function associated with Parkinson’s disease. It helps differentiate between neurogenic and non-neurogenic causes of urinary symptoms, enabling targeted interventions.
- Spinal Cord Injury: Urodynamic testing is crucial in patients with spinal cord injury to evaluate neurogenic bladder dysfunction. It provides critical information about bladder storage and emptying, helping guide interventions such as intermittent catheterization, medication, or surgical procedures.
- Stroke: Following a stroke, urodynamic testing helps determine the impact on bladder function and identify any neurogenic bladder dysfunction. It guides management strategies to improve bladder control and prevent complications such as urinary tract infections.
3. Pre- and Post-surgical Evaluation

Urodynamic testing is often employed as part of the pre-and post-surgical evaluation process in specific urologic procedures. It aids in assessing baseline bladder function and predicting post-operative outcomes:
- Prostate Surgery: Urodynamic testing helps evaluate bladder function before and after prostate surgery, such as transurethral resection of the prostate (TURP) or robotic-assisted prostatectomy. It helps identify any pre-existing bladder dysfunction and predicts the likelihood of post-operative urinary incontinence or urinary retention.
- Pelvic Organ Prolapse Surgery: Urodynamic evaluation assists in assessing bladder function in patients undergoing pelvic organ prolapse surgery, such as vaginal mesh repair or sacrocolpopexy. It helps identify any associated bladder dysfunction and guides management decisions.
- Sling Procedures for Incontinence: Urodynamic testing is crucial in evaluating bladder function before and after sling procedures, such as tension-free vaginal tape (TVT) or transobturator tape (TOT) placement. It helps assess urethral support and predicts post-operative outcomes, aiding in treatment planning.
Benefits of Urodynamic Testing

Urodynamic testing offers several benefits in the diagnosis and treatment of lower urinary tract disorders:
Accurate Diagnosis of Lower Urinary Tract Dysfunctions
Urodynamic testing provides valuable insights into the underlying causes of lower urinary tract dysfunctions. Assessing bladder capacity, pressure, and muscle activity, helps healthcare professionals accurately diagnose conditions such as overactive bladder, stress urinary incontinence, detrusor underactivity, and bladder outlet obstruction. This precise diagnosis allows for targeted treatment strategies, leading to more effective management.
Guiding Appropriate Treatment Options
The information obtained from urodynamic testing plays a vital role in selecting patients’ most appropriate treatment options. By identifying specific bladder dysfunctions, healthcare professionals can tailor interventions such as behavioral modifications, pelvic floor exercises, medications, minimally invasive procedures, or surgical interventions. This tailored approach maximizes the chances of successful treatment outcomes and improves patient satisfaction.
Monitoring Treatment Effectiveness
Urodynamic testing enables healthcare providers to monitor the effectiveness of chosen interventions over time. They can evaluate progress and make necessary adjustments by reassessing bladder function and dynamics after initiating treatment. This iterative process ensures that treatment plans are optimized for each patient, leading to improved outcomes and patient satisfaction.
Reducing the Risk of Complications and Improving Patient Outcomes
Accurate diagnosis and appropriate treatment selection through urodynamic testing help reduce the risk of complications associated with lower urinary tract disorders. By effectively managing conditions such as urinary incontinence, urinary retention, and bladder outlet obstruction, urodynamic testing helps prevent complications such as recurrent urinary tract infections, renal damage, and worsening of symptoms. This leads to improved patient outcomes, quality of life, and overall well-being.
Preparing for a Urodynamic Test

Proper preparation is crucial for obtaining accurate and reliable results during a urodynamic test. By following specific instructions, patients can ensure the effectiveness and validity of the testing process.
Patient Instructions and Expectations
Clear communication is essential to ensure patients understand the purpose, procedure, and potential discomfort associated with urodynamic testing. Healthcare professionals should provide detailed instructions, explain the expected duration of the test, and address any concerns or questions patients may have. This helps alleviate anxiety and ensures patient cooperation throughout the process.
Pre-test Procedures
Certain preparations may be necessary before undergoing a urodynamic test. These may include:
- Caffeine Restriction: Patients should be advised to avoid caffeine-containing beverages, such as coffee, tea, and soda, for a specified period before the test. Caffeine can affect bladder function and potentially interfere with test results.
- Bladder-Emptying Restrictions: Depending on the specific test being performed, patients may be instructed to arrive at the appointment with a comfortably full bladder or, in some cases, a partially empty bladder. Following these instructions is vital to obtain accurate measurements during the test.
Bladder Diary
Maintaining a bladder diary leading up to the urodynamic test provides valuable information about voiding habits, fluid intake, and urinary symptoms. Patients should be instructed to record the timing and volume of each void, any episodes of urinary incontinence, and any factors that may affect bladder function, such as fluid intake and activities. The bladder diary helps provide context to the urodynamic test results and assists healthcare professionals in their interpretation.
Medication Adjustments
In some cases, healthcare providers may recommend adjusting or temporarily discontinuing certain medications before the urodynamic test. This is particularly important for drugs affecting bladder function or interfering with test results. Patients should follow the specific instructions their healthcare provider provides regarding medication adjustments.
Hydration and Voiding Instructions
Patients may receive specific fluid intake and voiding instructions before the urodynamic test. They may be advised to drink a specified amount of fluids to ensure a comfortably full bladder for the test. Alternatively, in some cases, patients may need to follow instructions for partial bladder emptying before the test. Adhering to these instructions is crucial for accurate urodynamic test results.
Understanding Urodynamic Test Results

Interpreting urodynamic test results requires expertise. Different parameters and patterns indicate specific urodynamic diagnoses:
1. Normal vs. Abnormal Test Results
Healthcare professionals compare urodynamic test results against established normal ranges to determine abnormalities in bladder function. Normal test results indicate that the bladder and urinary system are functioning within the expected parameters. Abnormal test results may show underlying dysfunctions, such as bladder overactivity, underactivity, or obstruction.
2. Common Urodynamic Diagnoses
Urodynamic testing aids in diagnosing various conditions related to lower urinary tract dysfunction. Some common urodynamic diagnoses include:
- Detrusor Overactivity: Urodynamic test results showing involuntary bladder muscle contractions during filling may indicate detrusor overactivity, which can lead to symptoms such as urinary urgency and urge incontinence.
- Stress Urinary Incontinence: Urodynamic test results demonstrating urine leakage during activities that increase abdominal pressure, such as coughing or sneezing, may indicate stress urinary incontinence caused by weakened pelvic floor muscles.
- Detrusor Underactivity: Urodynamic test results showing reduced bladder contractility during voiding may suggest detrusor underactivity, characterized by incomplete bladder emptying and weak urine stream.
- Bladder Outlet Obstruction: Urodynamic test results indicating increased resistance to urine flow during voiding may suggest bladder outlet obstruction, which can be caused by conditions such as urethral strictures or an enlarged prostate.
3. Role of Urodynamic Findings in Treatment Planning
Urodynamic test results play a crucial role in guiding treatment planning. The specific findings inform healthcare professionals about the underlying bladder dysfunctions and help determine the most appropriate interventions.
Trust Your Urodynamic Healthcare Solutions to Us!

At Mobile Urodynamics Health Plus LLC
, we are committed to providing comprehensive and cutting-edge urodynamic healthcare solutions for accurately diagnosing and effectively treating lower urinary tract disorders. Our team of experienced medical professionals and state-of-the-art facilities ensure that patients receive the highest standard of care and personalized treatment plans tailored to their unique needs.
Contact us
today to discover how our expertise in urodynamic testing can make a difference in your healthcare journey. Our knowledgeable staff is ready to answer your questions, address your concerns, and schedule your urodynamic test. Trust us for reliable, accurate, and compassionate urologic care. Your optimal urinary health starts with us!