Pelvic Floor Dysfunction: Recognizing Symptoms and Effective Treatment Options

Pelvic floor dysfunction is a range of conditions affecting the pelvic region’s muscles, ligaments, and connective tissues. It can lead to various symptoms, such as urinary and bowel issues, as well as sexual dysfunction. Recognizing and addressing these symptoms is crucial for improving quality of life and seeking appropriate treatment options.
Understanding the Pelvic Floor
A complex network of muscles, ligaments, and tissues supports the organs within the pelvis, including the bladder, rectum, and uterus (in females). These muscles are vital in maintaining urinary and bowel control and sexual function. Pelvic floor dysfunction can occur whenever the pelvic floor is damaged or weakened.
A. Anatomy and Function of the Pelvic Floor Muscles
The pelvic floor muscles are divided into three layers: superficial, intermediate, and deep. The superficial muscles provide support to the openings of the urethra, vagina, and anus. The middle muscles help control urinary and bowel function, while the deep muscles stabilize the pelvis and provide structural support. Together, these muscles work to maintain continence, support the pelvic organs, and facilitate sexual function.
B. Role of the Pelvic Floor in Maintaining Urinary and Bowel Control
Maintaining bowel and urinary continence is the responsibility of the pelvic floor muscles. They work in coordination with the urinary and anal sphincters to control the flow of urine and feces. When these muscles contract, they tighten around the urethra and rectum, preventing leakage. Relaxing these muscles allows for urination and bowel movements. Any disruption or weakness in the pelvic floor muscles can lead to urinary or bowel incontinence.
C. Factors Contributing to Pelvic Floor Dysfunction
Pelvic floor dysfunction can be linked to numerous underlying factors. These may include pregnancy and childbirth, which can stretch and weaken the pelvic floor muscles. Hormonal changes during menopause can also affect the integrity of these muscles. Other risk factors include obesity, chronic constipation, repetitive heavy lifting, and certain medical conditions like pelvic organ prolapse or neurological disorders.
Recognizing Symptoms of Pelvic Floor Dysfunction

Recognizing the symptoms associated with pelvic floor dysfunction is crucial for timely intervention and appropriate treatment. Symptoms can manifest in various ways, affecting urinary, bowel, and sexual functions.
1. Urinary Symptoms
Urinary Incontinence: Weakening or dysfunction of the muscles supporting the pelvic organs can lead to involuntary urine leakage during activities such as coughing, sneezing, or exercising. This common symptom can significantly impact daily life and cause social discomfort.
- Frequent Urination: Even when the bladder is not completely filled, individuals may experience a frequent urge to urinate. This urge for frequent urination can disrupt daily activities and affect the quality of life.
- Urgency or Difficulty Initiating Urination: Some individuals may experience a strong urge to urinate even with a small amount of urine in the bladder. Others may have difficulty initiating urination or suffer from a weakened urinary stream, making urination more challenging and frustrating.
2. Bowel Symptoms
- Fecal Incontinence: Difficulty controlling bowel movements can result in unintentional leakage of feces. This symptom can cause distress and affect social interactions and self-confidence.
- Constipation or Difficulty Emptying the Bowels: Chronic constipation or difficulty fully emptying the bowels may be indicators of pelvic floor dysfunction. Infrequent bowel movements, a feeling of incomplete evacuation, and excessive straining can cause discomfort and affect overall bowel function.
- Rectal Pain or Discomfort: Persistent pain or discomfort in the rectal area, particularly during bowel movements, can be associated with pelvic floor dysfunction. This discomfort can interfere with daily activities and cause significant distress.
3. Sexual Symptoms
- Painful Intercourse (Dyspareunia): Pain or discomfort during sexual activity can be a sign of pelvic floor dysfunction. Increased muscle tension or spasms within the pelvic floor muscles may contribute to this symptom, impacting physical intimacy and emotional well-being.
- Erectile Dysfunction (in males): Pelvic floor dysfunction can contribute to difficulties in achieving or maintaining an erection. Weakened pelvic floor muscles can affect blood flow and nerve function, leading to erectile dysfunction and sexual dissatisfaction.
- Reduced Sexual Sensation: Weak pelvic floor muscles can reduce sexual sensation and pleasure for both males and females. This diminished sensitivity can affect sexual satisfaction and overall sexual well-being.
Diagnosis of Pelvic Floor Dysfunction

Accurate diagnosis of pelvic floor dysfunction involves a comprehensive evaluation, considering medical history, physical examination, and specific diagnostic tests.
A. Medical History and Physical Examination
During the medical history assessment, your healthcare provider will inquire about your symptoms, medical conditions, and any relevant factors that may contribute to pelvic floor dysfunction. A physical examination may involve an assessment of the pelvic region, including muscle tone and strength, as well as an evaluation of any pelvic organ prolapse.
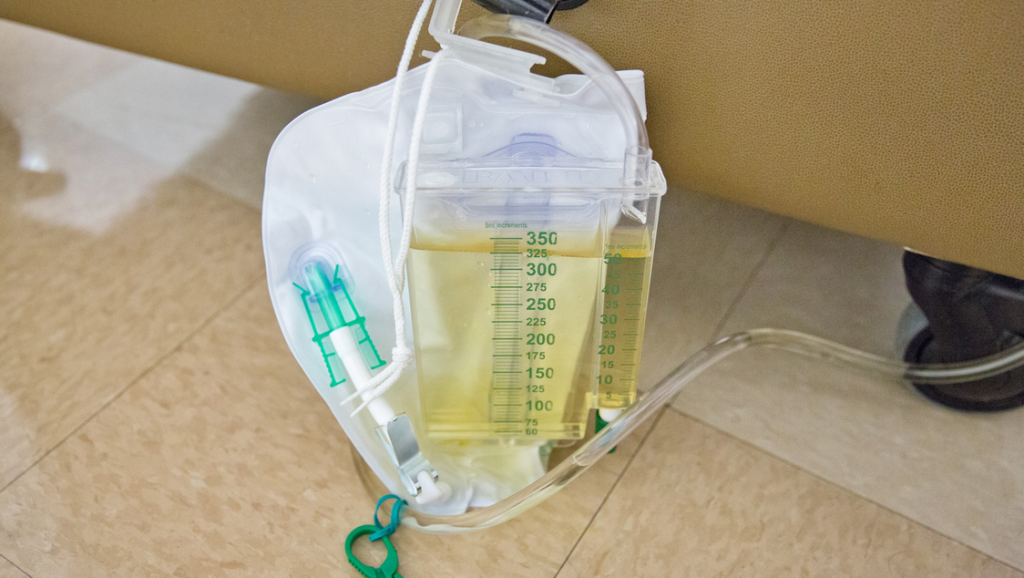
B. Urodynamic Testing
Urodynamic testing helps assess the function of the bladder, urethra, and pelvic floor muscles. Several types of urodynamic tests may be performed:
- Uroflowmetry: Measures the rate and volume of urine flow to evaluate voiding patterns.
- Cystometry: Measures bladder pressure during filling and emptying, providing information about bladder capacity and coordination.
- Pressure-Flow Study: Measures pressure in the bladder and urine flow rate simultaneously to diagnose bladder outlet obstruction.
- Electromyography (EMG): Measures electrical activity in the pelvic floor muscles to evaluate muscle function and coordination.
- Video Urodynamics: Combines urodynamic testing with real-time X-ray imaging to simultaneously assess bladder and pelvic floor function.
C. Other Diagnostic Tools (if applicable)
In some cases, additional diagnostic tools may be employed:
- Pelvic MRI or Ultrasound: Provides detailed images of the pelvic organs, muscles, and surrounding structures to evaluate abnormalities or pelvic floor damage.
- Endoscopy or Cystoscopy: Involves inserting a thin, flexible tube with a camera into the urethra or bladder to visualize the urinary tract and identify any structural or anatomical abnormalities.
Treatment Options for Pelvic Floor Dysfunction

The treatment of pelvic floor dysfunction aims to alleviate symptoms, improve muscle function, and enhance the quality of life. The choice of treatment depends on the specific symptoms and underlying causes.
A. Lifestyle Modifications
- Pelvic Floor Exercises (Kegels): These exercises involve contracting and relaxing the pelvic floor muscles to strengthen them and improve control.
- Dietary Changes: Adjusting your diet to include fiber-rich foods and maintaining proper hydration can help prevent constipation and promote regular bowel movements.
- Weight Management: Maintaining a healthy weight reduces pressure on the pelvic floor and may alleviate symptoms.
B. Behavioral Therapy
Bladder and Bowel Retraining: Establishing a regular schedule for urination and bowel movements helps retrain the bladder and bowel, improving control and reducing urgency.
Biofeedback: This technique uses sensors and visual or auditory cues to help individuals become aware of their pelvic floor muscles and learn how to control them effectively.
C. Medications
- Muscle Relaxants: Certain medications can help relax the pelvic floor muscles, reducing spasms and improving symptoms.
- Anticholinergics: These medications are used to reduce bladder overactivity and control urinary urgency.
- Topical Creams or Suppositories: Some topical treatments can help alleviate pain or discomfort associated with pelvic floor dysfunction.
Living with Pelvic Floor Dysfunction: Coping Strategies and Support

Living with pelvic floor dysfunction can be challenging, but there are strategies to cope with the condition and obtain support.
1. Emotional Impact and Psychological Support
The emotional impact of pelvic floor dysfunction should not be overlooked. Seeking support from healthcare professionals or joining support groups can provide emotional guidance and reassurance.
2. Pelvic Floor Physiotherapy
Pelvic floor physiotherapy, performed by specialized therapists, focuses on strengthening and rehabilitating the pelvic floor muscles through targeted exercises, manual techniques, and education on proper body mechanics.
3. Support Groups and Online Communities

Joining support groups or online communities dedicated to pelvic floor dysfunction can connect you with individuals experiencing similar challenges. Sharing experiences, advice, and tips can provide invaluable support and a sense of belonging.
Take Control of Your Pelvic Health Today
Don’t let pelvic floor dysfunction limit your quality of life any longer. At Mobile Urodynamics Health Plus LLC , we provide comprehensive urodynamic healthcare solutions tailored to your needs. Contact us today and regain control of your pelvic health.
Our experienced team offers state-of-the-art diagnostic tests and personalized treatment options for urinary, bowel, and sexual symptoms. With our mobile services, we bring convenience and privacy to your doorstep. Take the first step towards a better future—schedule an appointment with our compassionate team today!